Page 35 - NAPA 2021-2022
P. 35
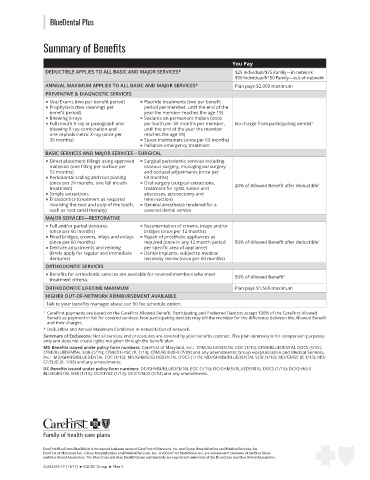
BlueDental Plus
Summary of Benefits
You Pay
DEDUCTIBLE APPLIES TO ALL BASIC AND MAJOR SERVICES* $25 Individual/$75 Family—in-network
$50 Individual/$150 Family—out-of-network
ANNUAL MAXIMUM APPLIES TO ALL BASIC AND MAJOR SERVICES* Plan pays $2,000 maximum
PREVENTIVE & DIAGNOSTIC SERVICES
■ ■ Oral Exams (two per benefit period) ■ ■ Fluoride treatments (two per benefit
■ ■ Prophylaxis (two cleanings per period per member, until the end of the
benefit period) year the member reaches the age 19)
■ ■ Bitewing X-rays ■ ■ Sealants on permanent molars (once
■ ■ Full mouth X-ray or panograph and per tooth per 36 months per member, No charge from participating dentist 1
bitewing X-ray combination and until the end of the year the member
one cephalometric X-ray (once per reaches the age 19)
36 months) ■ ■ Space maintainers (once per 60 months)
■ ■ Palliative emergency treatment
BASIC SERVICES AND MAJOR SERVICES—SURGICAL
■ ■ Direct placement fillings using approved ■ ■ Surgical periodontic services including
materials (one filling per surface per osseous surgery, mucogingival surgery
12 months) and occlusal adjustments (once per
■ ■ Periodontal scaling and root planing 60 months)
(once per 24 months, one full mouth ■ ■ Oral surgery (surgical extractions, 20% of Allowed Benefit after deductible 1
treatment) treatment for cysts, tumor and
■ ■ Simple extractions abscesses, apicoectomy and
■ ■ Endodontics (treatment as required hemi-section)
involving the root and pulp of the tooth, ■ ■ General anesthesia rendered for a
such as root canal therapy) covered dental service
MAJOR SERVICES—RESTORATIVE
■ Full and/or partial dentures ■ Recementation of crowns, inlays and/or
■ ■
(once per 60 months) bridges (once per 12 months)
■ Fixed bridges, crowns, inlays and onlays ■ Repair of prosthetic appliances as
■ ■
(once per 60 months) required (once in any 12 month period 50% of Allowed Benefit after deductible 1
■ Denture adjustments and relining per specific area of appliance)
■
(limits apply for regular and immediate ■ ■ Dental implants, subject to medical
dentures) necessity review (once per 60 months)
ORTHODONTIC SERVICES
■ Benefits for orthodontic services are available for covered members who meet
■ 50% of Allowed Benefit 1
treatment criteria.
ORTHODONTIC LIFETIME MAXIMUM Plan pays $1,500 maximum
HIGHER OUT-OF-NETWORK REIMBURSEMENT AVAILABLE
Talk to your benefits manager about our 90 fee schedule option.
1 CareFirst payments are based on the CareFirst Allowed Benefit. Participating and Preferred Dentists accept 100% of the CareFirst Allowed
Benefit as payment in full for covered services. Non-participating dentists may bill the member for the difference between the Allowed Benefit
and their charges.
* Deductible and Annual Maximum Combined In-network/Out-of-network.
Summary of Exclusions: Not all services and procedures are covered by your benefits contract. This plan summary is for comparison purposes
only and does not create rights not given through the benefit plan.
MD Benefits issued under policy form numbers: CareFirst of Maryland, Inc.: CFMI/BLUEDENTAL EOC (1/15); CFMI/BLUEDENTAL DOCS (1/15);
CFMI/BLUEDENTAL SOB (1/15); CFMI/51+/GC (R. 1/13); CFMI/ELIG/D-V (7/09) and any amendments; Group Hospitalization and Medical Services,
Inc.: MD/GHMSI/BLUEDENTAL EOC (1/15); MD/GHMSI/BLUEDENTAL DOCS (1/15); MD/GHMSI/BLUEDENTAL SOB (1/15); MD/CF/GC (R.1/13); MD/
CF/ELIG (R. 1/08) and any amendments;
DC Benefits issued under policy form numbers: DC/GHMSI/BLUEDENTAL EOC (1/15); DC/GHMSI/BLUEDENTAL DOCS (1/15); DC/GHMSI/
BLUEDENTAL SOB (1/15); DC/CF/GC (1/14); DC/CF/ELIG (1/14) and any amendments.
CareFirst BlueCross BlueShield is the shared business name of CareFirst of Maryland, Inc. and Group Hospitalization and Medical Services, Inc.
CareFirst of Maryland, Inc., Group Hospitalization and Medical Services, Inc., and CareFirst BlueChoice, Inc. are independent licensees of the Blue Cross
and Blue Shield Association. The Blue Cross and Blue Shield Names and Symbols are registered trademarks of the Blue Cross and Blue Shield Association.
SUM2596-1P (11/17) ■ MD/DC Group ■ Plan 5